Health Bulletin-July 2021

CANCER SCREENING
THE GLOBAL BURDEN OF CANCER
Worldwide:
In 2020, World Health Organization/International Agency for Research on Cancer estimated number of new cases and deaths worldwide are approximately 19.2 million and 9.96 million respectively and it is estimated to increase in cases by staggering 30.2 million and deaths by 16.3 million by 2040.
Top five common cancer types include breast, long, colorectal, prostate and stomach. Top five common cancer deaths are from lung, colorectal, liver, stomach and breast.
USA
In 2020, it was estimated about of I.8 million cancer cases and 606K cancer deaths that are expected to increase to 2.3 million and 952K, respectively. Overall, cancer death rate has been steadily decreasing since the 1990s and this decline is in large part by a dramatic decrease in the lung cancer death rate as a result of reduced smoking rates.
INDIA
In 2020, the estimated new cancer cases were 1.32M and all cancer deaths were 852K and these are estimated to increase to 2.09 million and 1.38 million respectively by 2040. Most common cancer cases include breast, lip and oral cavity, cervix uteri, lung, colorectal followed by esophageal and gastric. The most common cancer deaths follow the same order as new cases except colorectal is at the bottom among the above.
4 out of 10 cancer cases and half of all cancer deaths are associated with preventable modifiable risk factors. Therefore, lifestyle modifications such as quitting smoking and increasing physical activity can improve health outcomes in cancer patients and survivors.
- NOT using tobacco is the single best way a person can prevent cancer from developing.
- Nearly 20 percent of U.S. cancer diagnoses are related to excess body weight, alcohol intake, poor diet, and physical inactivity.
- Many cases of skin cancer could be prevented by protecting the skin from ultraviolet radiation from the sun and indoor tanning devices.
- Nearly all cases of cervical cancer could be prevented by HPV vaccination, but 49 percent of U.S. adolescents have not received the recommended doses of the vaccine.
WHAT IS CANCER SCREENING?
Screening for cancer means checking for precancerous lesions or cancer in people who have no signs or symptoms of the cancer for which they are being checked. The death rate from cervical cancer has fallen roughly 4% per year since the 1960’s with increased use of screening strategies.
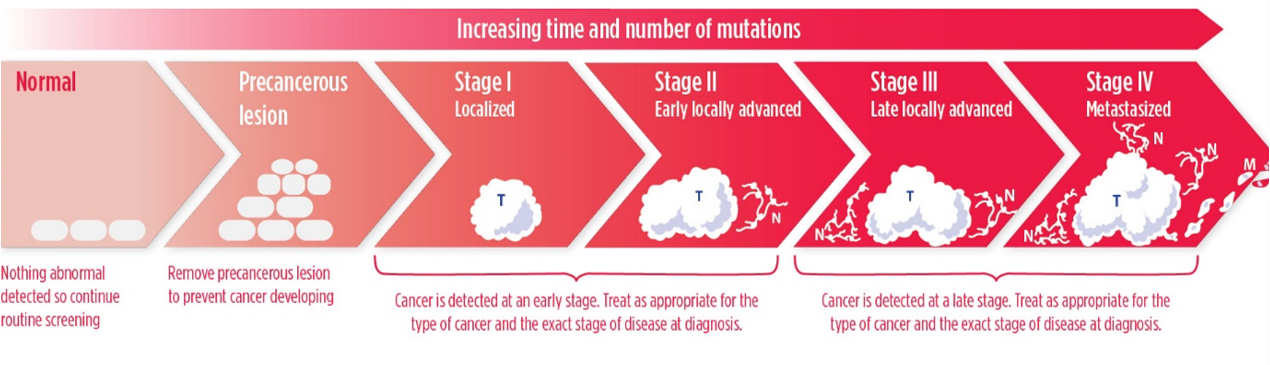
The aim is to find an abnormality at the earliest possible time in cancer development. If a cancer screening test shows a precancerous lesion is present, it can be treated or surgically removed before becoming cancer (See Figure). If a test finds an early stage I or II cancer, before it has spread, it is more likely that the patient can be treated successfully. For example, patients diagnosed with colorectal cancer or breast cancer when the cancer is confined to the colon or rectum, or to the breast, have 5-year relative survival rates of 90 percent and 99 percent, respectively, while those diagnosed with metastatic colorectal cancer or breast cancer, 5-year relative survival rates are decreased to 14 percent and 28 percent, respectively. Treating or surgically removing a precancerous lesion or early-stage cancer is called cancer interception.
HOW CAN WE SCREEN FOR CANCER?
Screening for cancer can be done in various ways, including by using imaging technologies to look for abnormalities inside the body, and by collecting tissue or fluid samples and then analyzing them for abnormalities characteristic of the cancer being screened for.
BREAST CANCER:
SCREENING MAMMOGRAM: Uses X-rays to image the breasts and the information that is generated can be stored on a film and is called as conventional mammogram or can be stored electronically and called as Digital mammography.
BREAST MRI (Magnetic Resonance Imaging): it uses radio waves and a powerful magnet to create detailed image of the breast.
Screening mammograms and MRI can detect breast cancer at any stage, but the aim is to detect cancer at the earliest possible stage.
CERVICAL CANCER:
PAP TEST: Samples cervical cells which are analyzed under the microscope for any abnormalities. It can detect precancerous or cancerous cervical lesions but the aim of the screening is to detect the cancer at the earliest possible stage.
HPV TEST: detects certain cervical cancer-causing types of human papilloma virus (HPV). This test does not directly detect precancerous or cancerous cervical lesions but identifies people for who further testing is recommended.
PROSTATE CANCER:
PSA TEST: it measures the protein in the blood called PSA (Prostate Specific Antigen). It does not directly detect the prostate cancer, but PSA is often elevated in men with prostate cancer. The test therefore identifies those men for whom further testing is warranted.
COLORECTAL CANCER:
STOOL TESTS: some tests detects the presence of red blood cells while others test both red blood cells and certain genetic mutations linked to colorectal cancer. these does not directly detect precancerous or cancer lesions but identifies people for whom further testing is recommended.
FLEXIBLE SIGMOIDOSCOPY AND COLONOSCOPY: both use flexible thin lighted tube with a small video camera on the end that allows the visualization of the lining of colorectal areas.
CT COLONOGRAPHY (VIRTUAL COLONOSCOPY): Uses X-rays to image the colon and rectum. Can detect precancerous or cancer appearing lesions and if such abnormalities are identified, a colonoscopy is recommended.
BLOOD TESTS: Detects epigenetic (“in addition to" the traditional genetic basis for inheritance and NOT related to DNA alterations) abnormalities, linked to colorectal cancer. These does not directly detect precancerous or cancer lesions but identifies people for whom further testing is recommended.
LUNG CANCER:
LOW DOSE CT SCAN: Uses low dose of X-Ray images. Can detect any stage cancer but aim of screening is to detect cancer at the earliest possible stage.
CONSENSUS ON CANCER SCREENING:
Ideal screening intervention should be widely available with low cost and low risk, more accurate and effective. Screening objective should be to reduce morbidity and the mortality of the screened disease and simply finding the disease at an earlier stage is NOT good enough if effective treatments are not available and does not result in reduced morbidity and mortality.
The benefits for cancer screening are 1) To find cancer early before it spreads and to lower the risk of death from cancer. For example, data showed that mammography screened women were 25 percent less likely to be diagnosed with advanced breast cancer. 2) To lower the cost of health care by reducing the need to treat cancer. 3) To maintain cancer awareness in the public.
The harms of screening are 1) Adverse events from procedure can still occur while the chances are low. 2) Anxiety while waiting on the results. 3) Falsely positive test results can lead unnecessary further interventions. 4) Falsely negative results would lead to missed opportunities for early treatment. 5) Over diagnosis can lead to over treatment and their related risks, as not all cancers detected early could go on to cause symptoms or threaten life.
COMPLETELY RIDICULOUS CANCER SCREENING TESTS:
Whole Body Scans such as CT, MRI, PET/CT and variety of blood Tumor Markers such as CEA, CA 125, CA19-9, CA 15-3, CA 27-29, SPEP, etc.
HOW DO I KNOW IF I AM AT INCREASED RISK OF INHERITED CANCER?
If a person has a) personal or family history of cancer at a younger age in their 20’s, b) >1 cancer such as Breast/Ovarian, colon/endometrial, c) in both of paired organs such eyes, kidneys, breasts, d) multiple first degree relatives or several family with same cancer, e) male breast cancer, f) congenital birth defects, g) high risk racial/ethnic such as Ashkenazi Jews; These individuals should consult a health care provider and consider genetic testing and if positive to discuss risk-reducing measures for them.
SCREENING GUIDELINES:
BREAST CANCER SCREENING:
There is consensus among professional societies that women ages 50-74 who are at average risk of developing breast cancer should have regular screening mammograms. However, the variability about whether this should be done every year or every other year. Some organizations recommend screening mammograms for average risk women should be performed at either age 40 or 45. It is important to note, however, then all the groups support women ages 40 to 49 having the opportunity to have regular screening mammograms if they decide it is right for them.
CERVICAL CANCER SCREENING:
There is consensus among the professional societies that
- Average risk women younger than 21 should not be screened.
- Average risk women ages 21 to 29 should have PAP test every 3 years. ACS recommends from age 25.
- Average risk women ages 32- 65 should have either Pap test alone every 3 years or PAP with HPV every 5 years or HPV alone every 5 years.
- No screening for Women older than 65 if their previous test results were normal and are not otherwise at high risk and for those who had a total hysterectomy for benign disease.
PROSTATE CANCER:
There is consensus among the professional societies that men ages 55 to 69 who are at average risk of developing prostate cancer talk to a physician about benefits and potential harms of PSA testing before deciding if screen is right for them.
COLORECTAL CANCER (CRC) SCREENING:
USPSTF has now updated the recommendation because of rising incidence in younger than 50 years, that individuals at average risk, begin screening at age 45 instead of age 50. This aligns with ACS 2018 recommendation of initiating screening at age 45.
NCCN and MSTF recommend that individuals at increased risk because of inherited Lynch syndrome should start screening with colonoscopy every one to two years at age 20-25 or 2-5 years prior to the youngest case in the immediate family if it was diagnosed before age 25.
ACS, NCCN, MSTF recommend that individuals at increased risk because they have a first degree relative who has been diagnosed with CRC should start screening with colonoscopy at age 40 or 10 years before the youngest case was diagnosed whichever is earlier.
LUNG CANCER:
There is consensus among the ACS, NCCN, and USPS TF that annual screening with low dose CT should be limited to adults ages 55 to 80 who are at high risk for lung cancer, and these include who smoked cigarettes at least one pack per day for 30 years, or 2 packs/day for 15 years, actively smoking or have quit within the past 15 years. USPSTF is currently reviewing whether screening should begin at an earlier age and include with < 30 pack years smoking.
ACRONYMS
USPSTF - US Preventive Services Task Force, ACS – American Cancer Society, NCCN – National Comprehensive Cancer Network, MSTF – Multi Society Task Force
Resources:
Globocan-WHO-International Agency for Research on Cancer; American Association of Cancer Research and National Cancer Institute.
Contributed By- Venu G Bathini, MD
Program Director, Hematology Oncology Fellowship
Associate Professor, Department of Medicine, UMass Medical School
Division of Hematology & Oncology
Univ of Massachusetts Memorial Medical Center
Worcester, MA 01545
Coordinated By
Sujeeth R. Punnam, MD
Chair, Health Committee
(Dr. Sujeeth R. Punnam is a cardiologist in Stockton, California and is affiliated with multiple hospitals in the area, including Dameron Hospital and St. Joseph's Medical Center-Stockton. He received his medical degree from Kakatiya Medical College NTR and has been in practice for more than 20 years.)

 Join our
Join our